Introduction
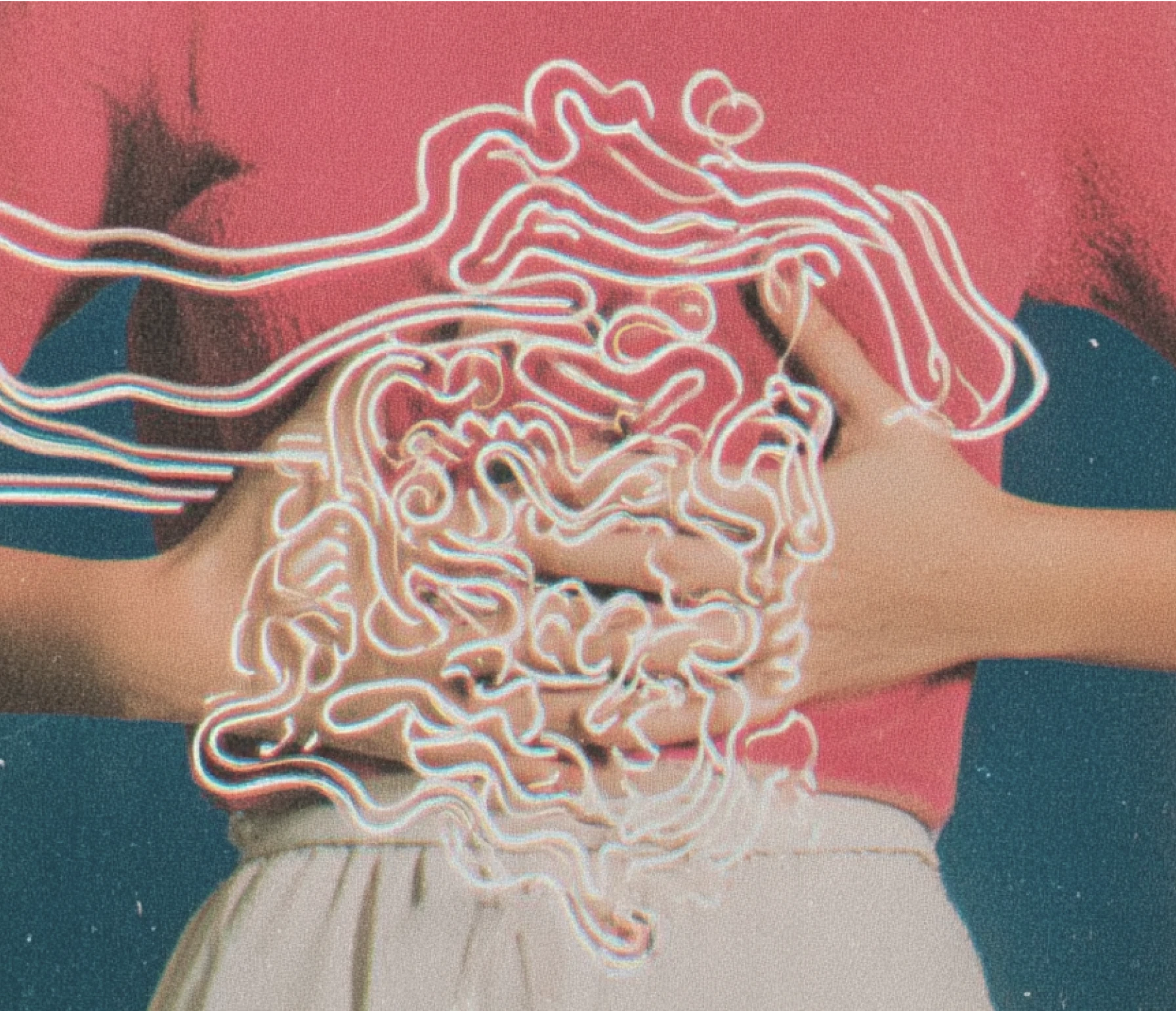
Do you often struggle with stomachaches, bloating, or digestive discomfort? Do you wonder why these issues persist despite your efforts to eat healthily and exercise? You’re not alone. Gut health problems are increasingly common, yet their root causes and solutions remain a mystery to many. This guide aims to change that.
Purpose of the guide
Gut Health 101 is designed to demystify the complex world of the gut and provide actionable insights for improving its overall well-being. This guide delves into common gut health issues, their root causes, and influencing factors, such as diet, lifestyle, and the environment. It provides practical strategies for healing and maintaining a healthy digestive system and understanding gut health from a root-cause perspective.
Gut health is not just about avoiding discomfort; it’s about the underlying factors that contribute to a healthy gut. From diet and lifestyle to environmental influences and medications, numerous things can impact the gut microbiome and overall digestive health. By addressing these root causes, lasting improvements can be enacted.
This guide provides a comprehensive look at gut health, detailing the microbiome, leaky gut, and effective healing strategies. It begins by defining the microbiome and its vital roles in digestion, immune function, and mood regulation. It then explores how dysbiosis and leaky gut syndrome contribute to chronic inflammation and various systemic issues, including digestive, immune, skin, mental, cardiovascular, metabolic, hormonal, musculoskeletal, and cancer-related problems.
The guide offers practical strategies for gut healing, including dietary adjustments, probiotics, supplements, lifestyle changes, and personalized care approaches according to the 5R framework for a root-cause approach.
Importance of the Gut Microbiome in Overall Health
Imagine a bustling city within the body, teeming with trillions of microscopic residents—this is the gut microbiome. These vibrant communities of beneficial bacteria, viruses, and fungi play key roles in digestion, immune defense, and even mental health. A well-balanced gut microbiome acts like a skilled team, ensuring smooth digestion, bolstering the immune system, enhancing mental clarity through the gut-brain connection, and lowering the risk of chronic diseases such as diabetes, obesity, and cardiovascular disease by modulating inflammation and improving metabolic health.1
Epidemiology of gut issues
When this microbial community falls into disarray, gut health issues arise. These conditions are more common than you might think and can significantly impact quality of life. For instance:
- Irritable bowel syndrome (IBS): A gastrointestinal disorder characterized by chronic abdominal pain, bloating, and altered bowel habits.2 It affects about 10–15% of the global population.3
- Inflammatory bowel disease (IBD): Includes Crohn’s disease and ulcerative colitis, affecting approximately 1.6 million Americans.4 Severe inflammation in the digestive tract with these conditions can cause extreme digestive issues and inflammatory issues in other areas of the body.5
- Intestinal permeability/leaky gut syndrome: This common and increasingly recognized condition is linked to a variety of health problems due to increased intestinal permeability or leakiness that allows toxins and bacteria to enter the bloodstream. When undigested food particles and toxins enter the bloodstream, it can lead to systemic inflammation and immune system activation, contributing to autoimmune diseases, chronic inflammatory disorders, and metabolic disturbances.6
- Gastroesophageal reflux disease (GERD): A chronic condition where stomach acid frequently flows back into the esophagus, causing irritation. It affects about 20% of the Western population.7
- Celiac disease: An autoimmune disorder triggered by gluten, leading to damage in the small intestine. It affects roughly 1% of people worldwide.8
- Diverticulitis: Inflammation or infection of small pouches that can form in the walls of the digestive tract, most commonly in the colon. It affects about 200,000 people in the United States each year, with over 50% of people over the age of 60 and over 60% of people over age 80 impacted by diverticulitis.9
Understanding the prevalence and impact of these conditions highlights the essential importance of maintaining a healthy gut microbiome and strong intestinal lining.
Gut health for life
Optimizing gut health is linked to extending health span, the period of life spent in good health.10 Studies indicate that a healthy gut can enhance health span by reducing inflammation and improving metabolic functions.11 Gut health plays a central role in chronic disease risk, as an imbalance in the gut microbiome and increased intestinal permeability can contribute to systemic inflammation and immune dysregulation. This dysregulation is linked to various chronic conditions, including cardiovascular disease, diabetes, and autoimmune disorders.12
The gut-brain axis influences cognitive health, and optimizing gut health can reduce the risk of neurodegenerative disorders by decreasing neuroinflammation and improving neurotransmitter function.13 A healthy gut also supports athletic and work performance by improving nutrient absorption, reducing inflammation, and enhancing mental clarity and focus.14 And a well-functioning gut microbiome can increase energy levels and promote a sense of vibrancy by optimizing nutrient absorption and reducing systemic inflammation.15,16
Microbiome definition and composition
The microbiome represents an intricate ecosystem of microorganisms living inside the human body.17 Within the gastrointestinal tract, this diverse community includes bacteria, archaea, fungi, and viruses, all of which play essential roles in maintaining health and influencing disease.18 Understanding the composition and functions of these microbial populations provides insight into their significant impact on human physiology and well-being.
The human body contains approximately 30 trillion human cells, but the gut alone hosts around 100 trillion microbial cells, highlighting microbial dominance in terms of cell count.19 The microbiome harbors over three million unique genes, vastly outnumbering the approximately 20,000 human genes by almost 150 times. This microbial gene pool contributes to various metabolic processes and the synthesis of essential metabolites.20
The gastrointestinal tract (GI) tract harbors a complex and dynamic microbial ecosystem:
- Bacteria: Major phyla such as Firmicutes, Bacteroidetes, Actinobacteria, and Proteobacteria are essential for digestion, immune modulation, and synthesis of certain vitamins.21 These microbes perform various functions, including:
- Digesting complex carbohydrates: Breaking down fiber to produce short-chain fatty acids (SCFAs), which are needed for gut health.22
- Synthesis of vitamins: Producing vitamins such as B12, folate, and K.23
- Immune system modulation: Influencing immune responses and protecting against pathogenic microbes.24
- Archaea: Microbes like methanogens are mainly involved in the production of methane and hydrogen, which are byproducts of microbial fermentation.25
- Fungi: Yeasts like Candida and Saccharomyces contribute to the microbiome balance, play a role in nutrient metabolism, and contribute to the overall microbial balance.26
- Viruses: Including bacteriophages that interact with bacteria and potentially influence microbial community dynamics.27
The microbiome’s contribution: Functions of the gut microbiome
The community of microorganisms living in the GI tract performs several pivotal functions that are essential for overall health.28 Here’s a look at some of the key roles it plays:
Digestion and nutrient absorption
One of the primary functions of the gut microbiome is aiding in digestion and nutrient absorption. The microorganisms in the gut help break down complex carbohydrates and fibers from the diet that digestive enzymes can’t handle.29 They convert these fibers into short-chain fatty acids (SCFAs), which cells then use as energy sources. This process also helps absorb nutrients, ensuring that the body gets the vitamins and minerals it needs to function properly.30
Production of essential metabolites
The microorganisms in the gut also produce essential metabolites, including vitamins and hormones. For example, certain bacteria help produce B vitamins, vitamin K, and other compounds that are important for health. These metabolites play roles in various bodily functions, such as blood clotting, energy production, and maintaining the health of our skin and bones.
Around one-third to one-half of the metabolites in the blood come from the microbiome. These include:
- Short-chain fatty acids (SCFAs): Acetate, propionate, and butyrate, which are important for energy production and maintaining gut health.31
- Vitamins: B vitamins and vitamin K, which are needed for various bodily functions.23
- Hormones and neurotransmitters: Produced or influenced by the microbiome, affecting mood and mental health.32
Immune system interaction
The gut microbiome also plays a significant role in regulating the immune system. The microorganisms in the gut help train and balance the immune response, making sure that the immune system reacts appropriately to harmful invaders while avoiding unnecessary attacks on the body’s own tissues. A healthy microbiome supports the production of antibodies and other immune cells, helping to protect from infections and diseases.33
Second brain
Interestingly, the gut microbiome is often referred to as the “second brain” because of its influence on mood and mental health. The gut and the brain communicate through a complex network known as the gut-brain axis.34 The microbiome produces neurotransmitters and other chemicals that can affect mood, stress levels, and overall mental well-being.35 This connection shows how closely digestive health can be linked to mental health (see Mental Health 101 and Stress Management 101).
Gut-Immune System Interaction
The gut microbiome plays a pivotal role in interacting with and regulating the immune system. It is both complex and vital for maintaining overall health and immune balance.33
Interaction between microbiome and immune system
The microorganisms in the gut are in constant communication with the immune system. This collaboration helps regulate immune responses, ensuring that the body can effectively defend against pathogens while maintaining tolerance to non-harmful antigens.36
Immune regulation by gut bacteria
Gut bacteria help develop and train immune cells, such as T cells, to respond appropriately to threats. By producing metabolites like short-chain fatty acids (SCFAs), gut bacteria influence the activity and differentiation of these immune cells, promoting a balanced immune response.37
Role in pathogen defense and immune tolerance
Microbes in the gut microbiome are involved in both defending against pathogens and promoting immune tolerance. The microbiome helps prevent infections by competing with harmful microbes for resources and space in the gut. Additionally, it produces antimicrobial substances that directly inhibit pathogen growth. Simultaneously, the microbiome teaches the immune system to tolerate harmless substances, reducing the risk of unnecessary immune responses.38
Impact of a healthy microbiome on immune balance
A healthy gut microbiome is critical for maintaining immune homeostasis, the state of balanced immune function. When the microbiome is diverse and balanced, it supports the immune system in distinguishing between harmful and harmless entities and regulates the production of anti-inflammatory and pro-inflammatory signals. These signals help the immune system respond proportionately to threats, preventing excessive inflammation that can lead to tissue damage.39
Prevention of autoimmune responses
A well-balanced microbiome helps prevent chronic inflammation and keeps the immune system from overreacting to non-threatening substances. A balanced gut microbiome helps the immune system develop tolerance to the body’s own tissues, reducing the risk of autoimmune diseases where the immune system mistakenly attacks healthy cells. By supporting regulatory T cells and other mechanisms of immune tolerance, the microbiome helps maintain self-tolerance and prevent autoimmunity.38
Dysbiosis: Imbalance in Gut Bacteria
Dysbiosis occurs when the balance of microorganisms in the gut becomes disrupted.40 This imbalance can affect health in several ways and is linked to a range of conditions.
Causes of dysbiosis
Several factors can cause this imbalance:
- Diet: Eating a lot of processed foods or high sugar levels can disturb the gut microbiome.41
- Alcohol consumption: The gut microbiome can be altered by even moderate alcohol intake.42
- Antibiotics and other medications: These can kill both harmful and beneficial bacteria, leading to an imbalance.43
- Toxins: Exposure to environmental toxins, such as air pollutants, chemicals in plastics, and pesticides, can affect gut health.44
- Infections: Infections or overgrowths of harmful microbes can disrupt the microbiome.37
- Stress: High levels of stress can negatively impact the gut microbiome45 (see Mental Health 101 and Stress Management 101).
- C-section delivery and lack of breast milk: Babies delivered vaginally and those who are breastfed are exposed to beneficial bacteria from their mother’s birth canal and breast milk. C-section-delivered babies and those who are not breastfed might miss those beneficial bacteria. This exposure helps establish a healthy gut microbiome early in life, promoting balanced bacterial populations and supporting overall immune development and health.46
Impact on health of dysbiosis
When dysbiosis occurs, the balance of bacteria in the gut gets thrown off. This can lead to fewer beneficial bacteria and more harmful ones. As a result, the gut’s ability to perform its functions, such as digesting food and supporting the immune system, may be compromised.
Dysbiosis can lead to various health issues:
- Immune system imbalance: An imbalance in gut bacteria can cause immune cells to become overactive, leading to chronic inflammation and health problems.39
- Immune system confusion: The immune system may become confused and start attacking the body’s own tissues, leading to autoimmune diseases like rheumatoid arthritis or lupus.38
- Molecular mimicry: This is when the immune system mistakes the body’s own cells for harmful invaders due to similarities in the molecular structure, which can trigger autoimmune responses.47
- Inflammation: Changes in the types of metabolites produced by gut bacteria can lead to inflammation throughout the body.48
- Metabolite imbalances: When dysbiosis occurs, the production of metabolites—including short-chain fatty acids (SCFAs) that help fuel gut cells, vitamins like B vitamins and vitamin K, and hormones that influence mood and metabolism—can be disrupted, affecting overall health. For instance, fewer SCFAs can lead to reduced energy levels and poor gut health, while changes in vitamin levels can impact various bodily functions.48
Maintaining a balanced gut microbiome is essential for overall health, as it influences digestion, immune function, and many other biological processes. Dysbiosis can lead to a range of health issues, from inflammation and immune system problems to broader impacts on overall well-being.
Intestinal Barrier Dysfunction/Leaky Gut Syndrome
Intestinal barrier dysfunction, commonly known as leaky gut syndrome, occurs when the lining of the small intestine becomes damaged, allowing harmful substances to pass through into the bloodstream.49 Imagine the gut lining as a finely woven net that allows only beneficial nutrients to pass through while keeping harmful substances out. When this net gets torn, harmful substances like toxins and undigested food particles slip into the bloodstream, potentially causing a cascade of health issues. A major culprit behind this condition is dysbiosis, which is an imbalance in the gut bacteria. This imbalance and the resulting leaky gut can affect multiple systems in the body, leading to a wide range of symptoms and diseases.50
Causes of intestinal barrier dysfunction/leaky gut syndrome
Factors contributing to the increased intestinal permeability that occurs with a leaky gut include:
- Poor diet: Diets high in fat, sugar, and processed foods and low in healthy fibers can disrupt the gut barrier by promoting inflammation, altering the gut microbiota, and damaging the intestinal lining.51
- Alcohol consumption: The gut microbiome can be altered by even moderate alcohol intake.42
- Medications: Prolonged use of antibiotics,52 non-steroidal anti-inflammatory drugs (NSAIDs),53 and other medications can disrupt the gut microbiome and damage the intestinal lining.
- Toxins: Exposure to environmental toxins and pollutants can damage the gut lining, disrupt the balance of gut bacteria, and increase intestinal permeability.54
- Infections: Bacterial, viral, or fungal infections can increase inflammation and disrupt the gut lining.55
- Stress: Chronic stress can negatively impact gut health by altering the gut microbiota and weakening the intestinal barrier56 (see Mental Health 101 and Stress Management 101).
- Allergens: Food allergies and sensitivities can trigger inflammation57 and damage the gut lining.
When the gut lining is disrupted, it loses its ability to effectively act as a barrier. This allows undigested food particles, toxins, and harmful bacteria to leak into the bloodstream, triggering an immune response.58
Impact on health of intestinal barrier dysfunction/leaky gut syndrome
The escape of harmful substances into the bloodstream can lead to widespread health issues. The immune system reacts to these invaders, potentially causing inflammation and tissue damage throughout the body.58 This immune reaction can lead to the following, which can then cause widespread health issues elsewhere if not addressed.
- Digestive issues: Increased intestinal permeability can lead to symptoms such as bloating, gas, cramps, diarrhea, and constipation by allowing harmful substances to enter the gut and cause inflammation.59
- Nutrient malabsorption: Leaky gut can impair the absorption of essential nutrients, resulting in deficiencies that affect overall health and energy levels .60
- Autoimmune diseases: Leaky gut is linked to the development of autoimmune diseases like rheumatoid arthritis and lupus, as the immune system starts attacking the body’s own tissues.61
- Chronic inflammation: The passage of toxins and pathogens into the bloodstream can trigger chronic inflammation, which is associated with various chronic diseases, including mental health and cognitive issues, heart disease, and diabetes.6
Systems Impacted by Dysbiosis/Leaky Gut
Digestive (gastrointestinal) system
Dysbiosis and leaky gut play a significant role in the development of various gastrointestinal diseases. When the balance of gut bacteria is disrupted and the intestinal lining becomes permeable, it leads to inflammation and immune responses that can damage the digestive system.62
Specific gastrointestinal diseases associated with dysbiosis and leaky gut:
- Irritable bowel syndrome (IBS): Dysbiosis is frequently observed in IBS patients, leading to symptoms like abdominal pain, bloating, and altered bowel habits.63
- Inflammatory bowel disease (IBD): Conditions such as Crohn’s disease and ulcerative colitis are linked to both dysbiosis and increased intestinal permeability, causing chronic inflammation of the digestive tract.64
- Celiac disease: Leaky gut can allow gluten peptides to cross the intestinal barrier, triggering an autoimmune response in genetically predisposed individuals.65
- Small intestinal bacterial overgrowth (SIBO): An overgrowth of bacteria in the small intestine can result from dysbiosis, leading to symptoms like bloating, diarrhea, and malabsorption.66
- Small intestinal fungal overgrowth (SIFO): A condition characterized by an excessive proliferation of fungi, predominantly from the Candida genus, in the small intestine that causes digestive issues such as bloating and abdominal pain; systemic symptoms like fatigue, skin problems, and increased food sensitivities; and is often accompanied by mental health symptoms like brain fog.67
- Non-alcoholic fatty liver disease (NAFLD): Dysbiosis and leaky gut contribute to NAFLD by allowing endotoxins to enter the bloodstream and promote liver inflammation and fat accumulation.68
Immune system
The immune system is responsible for protecting the body from infections and harmful substances. When foreign substances enter the bloodstream through a leaky gut, they can trigger inappropriate immune responses.69 This leads to chronic inflammation and increases the risk of developing various immune-related diseases.6
Continuous exposure to inflammatory triggers from the gut can lead to systemic inflammation, which is associated with various chronic diseases.70 Dysbiosis and leaky gut are also linked to an increased risk of autoimmune diseases, where the immune system mistakenly attacks the body’s own tissues.61
Specific immune diseases associated with dysbiosis and leaky gut:
- Rheumatoid arthritis: Increased intestinal permeability and dysbiosis have been associated with rheumatoid arthritis, as the immune system may attack joint tissues in response to gut-derived inflammatory signals.71
- Lupus: Systemic lupus erythematosus (SLE) has been linked to leaky gut, where immune responses to gut antigens contribute to autoimmune reactions.72
- Celiac disease: In individuals with celiac disease, leaky gut allows gluten proteins to trigger an autoimmune response, leading to damage in the small intestine.73
- Type 1 diabetes: Dysbiosis and increased intestinal permeability have been implicated in the development of type 1 diabetes through immune system dysfunction and autoimmune responses.74
Skin
The skin is the body’s largest organ and serves as a barrier to protect against external threats. Dysbiosis and leaky gut can impact skin health by causing systemic inflammation and immune system dysfunction. When the gut lining is compromised, inflammatory signals and toxins can spread throughout the body, affecting the skin and leading to various dermatological conditions.75
Specific skin diseases associated with dysbiosis and leaky gut:
- Eczema (atopic dermatitis): Eczema is linked to increased intestinal permeability and dysbiosis,76 where gut-derived inflammatory factors contribute to skin inflammation and itching.77
- Psoriasis: This autoimmune skin condition, characterized by red, scaly patches, has been associated with dysbiosis and leaky gut, as systemic inflammation can exacerbate symptoms.78
- Acne: Acne has been connected to gut health, with leaky gut and dysbiosis potentially contributing to systemic inflammation and hormonal imbalances that worsen acne.79
Brain health (neurology)
The brain and the gut are closely connected through the gut-brain axis,80 a communication network where the gut and brain constantly exchange signals, influencing everything from mood and emotions to cognitive function and overall mental health.81 Dysbiosis and leaky gut can impact brain health by causing systemic inflammation and disrupting neurotransmitter production.82 When the gut barrier is compromised, inflammatory signals can affect the brain, contributing to various neurological and psychiatric conditions.83
Specific brain health issues associated with dysbiosis and leaky gut:
- Brain fog/cognitive dysfunction: A state characterized by confusion, forgetfulness, and lack of focus and mental clarity. An imbalanced gut microbiome can lead to increased intestinal permeability or leaky gut, allowing toxins to enter the bloodstream and reach the brain. This can result in inflammation and cognitive impairments, commonly referred to as brain fog.84
- Alzheimer’s disease: Chronic inflammation and immune responses triggered by leaky gut can impair cognitive function, leading to memory issues and potentially contributing to neurodegenerative diseases such as Alzheimer’s.85
Gut and mind (psychiatry)
Nutritional psychiatry explores how diet influences mental health, with research showing that imbalances in gut microbiota and compromised gut barrier function, often referred to as “leaky gut,” can significantly affect mood and contribute to conditions like depression and anxiety.86 This is because the gut microbiome plays an important role in regulating inflammation and neurotransmitter production, both of which are essential for maintaining emotional balance32 (see Nutrition 101).
Specific mental health issues associated with dysbiosis and leaky gut:
- Depression: Dysbiosis and leaky gut can lead to increased systemic inflammation and influence neurotransmitter production,82 which affects brain function and mood regulation.32 Dysbiosis and leaky gut are linked to depression, as gut-derived inflammatory cytokines can influence brain chemistry and mood.87
- Anxiety disorders: Increased intestinal permeability and systemic inflammation have been associated with anxiety disorders, affecting the brain’s response to stress.88
- Bipolar disorder: A mental health condition characterized by extreme mood swings, including emotional highs (mania) and lows (depression). Dysbiosis may exacerbate inflammation and affect neurotransmitter balance, potentially influencing mood and behavior and impacting the severity of bipolar disorder symptoms.89
- Autism spectrum disorder (ASD): A developmental disorder that affects communication and behavior. Children with ASD often exhibit gastrointestinal issues, and dysbiosis is commonly observed in these individuals. The gut microbiome can affect brain development and function, contributing to the symptoms of autism.90
- Attention-deficit/hyperactivity disorder (ADHD): A neurological disorder marked by an ongoing pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development. Dysbiosis might influence the production of neurotransmitters such as dopamine and serotonin, which are essential for attention and behavior regulation. Altered gut bacteria have been associated with ADHD symptoms.91
- Schizophrenia: A chronic and severe mental disorder affecting how a person thinks, feels, and behaves, often characterized by hallucinations and delusions. Dysbiosis has been linked to schizophrenia through its influence on the gut-brain axis, potentially exacerbating inflammation and altering neurotransmitter production, which can contribute to the symptoms of schizophrenia. Emerging research suggests that gut microbiota imbalances may impact brain function and behavior, providing a potential avenue for understanding and managing this complex disorder.92
Cardiovascular
Cardiovascular health is significantly influenced by gut health. Inflammation is a key factor in the development of various cardiovascular diseases.93 Risk factors include dysbiosis, leaky gut, poor diet, sedentary lifestyle, and genetic predispositions.
Specific diseases associated with dysbiosis and leaky gut:
- Atherosclerosis: Chronic inflammation from leaky gut contributes to the buildup of plaques in arteries, increasing the risk of heart attacks and strokes.94
- Hypertension (high blood pressure): Dysbiosis and systemic inflammation can lead to increased blood pressure, further straining the cardiovascular system.95
- Heart failure: Inflammatory responses linked to dysbiosis and leaky gut are associated with an increased risk of heart failure.96
Metabolic
Metabolic health is closely tied to gut health, with the balance of gut bacteria playing a key role in managing weight, blood sugar, and overall metabolic function.97 Dysbiosis and leaky gut can lead to systemic inflammation and metabolic dysfunction, increasing the risk of various metabolic disorders.98 Diet, physical activity, environmental exposures, and genetic predispositions influence gut and metabolic health.
Impact of dysbiosis and leaky gut on metabolic issues:
- Obesity: An imbalanced gut microbiome can affect energy balance and metabolism, leading to weight gain and obesity. Inflammation and immune activation from dysbiosis can disrupt normal metabolic processes and fat storage.99 Additionally, the increased permeability of the gut allows endotoxins to enter the bloodstream, further exacerbating inflammation and metabolic imbalances that drive obesity and associated insulin resistance100 (see Weight Management 101).
- Lipid metabolism: Dysbiosis can alter the metabolism of lipids, leading to dyslipidemia, which involves abnormal levels of cholesterol and triglycerides.101 Chronic inflammation contributes to the development of metabolic syndrome.98
- Non-alcoholic fatty liver disease (NAFLD): Leaky gut can allow endotoxins to reach the liver, causing inflammation and fat accumulation.68 Dysbiosis and chronic inflammation are linked to the progression of NAFLD.102
Specific diseases associated with dysbiosis and leaky gut:
- Insulin resistance: Chronic inflammation from leaky gut can disrupt insulin signaling pathways, contributing to insulin resistance—a condition where the body’s cells do not respond effectively to insulin, leading to elevated blood sugar levels.103
- Type 2 diabetes: Over time, insulin resistance induced by inflammation and increased gut permeability causes the pancreas to produce more insulin to compensate, eventually resulting in high blood sugar levels when the pancreas can no longer keep up, leading to type 2 diabetes.103 In addition, an imbalanced gut microbiome can lead to increased inflammation and disrupt the secretion of hormones like GLP-1, which plays a role in insulin sensitivity and glucose metabolism.104
- Dyslipidemia: An altered gut microbiome can disrupt lipid metabolism, resulting in abnormal cholesterol and triglyceride levels.101
- Metabolic syndrome: Chronic inflammation from leaky gut contributes to the cluster of conditions that constitutes metabolic syndrome, including high blood pressure, abnormal cholesterol levels, and excess body fat.105
Hormone (endocrine)
Dysbiosis and leaky gut can significantly impact endocrine health by causing chronic inflammation and disrupting the delicate balance of hormone regulation.
Specific diseases associated with dysbiosis and leaky gut:
- Hashimoto’s thyroiditis: Dysbiosis can contribute to thyroid dysfunction by promoting autoimmune responses and inflammation, which may lead to conditions like Hashimoto’s thyroiditis, an autoimmune disorder where the immune system attacks the thyroid gland, leading to hypothyroidism and an underactive thyroid.106
- Adrenal issues: Dysbiosis impacts the adrenal glands by triggering chronic inflammation and stress responses, which can disrupt the balance of hormones produced by the adrenal glands.107 Gut imbalances lead to increased levels of systemic inflammation, which overburdens the adrenal glands and impairs their ability to regulate stress and produce hormones effectively.108 This can overwhelm the adrenal glands, leading to low energy, chronic fatigue, and difficulty managing stress.
- Polycystic ovary syndrome (PCOS): Altered gut microbiota and systemic inflammation can influence hormone imbalances associated with PCOS, affecting menstrual cycles and fertility.109
Musculoskeletal
Dysbiosis and leaky gut can lead to musculoskeletal problems, primarily through chronic inflammation. When the gut lining is compromised, inflammatory molecules and endotoxins can enter the bloodstream, causing systemic inflammation that affects joints and tissues.110 This inflammation can exacerbate or contribute to various musculoskeletal disorders.
Specific diseases associated with dysbiosis and leaky gut:
- Rheumatoid arthritis (RA): RA is an autoimmune disease affecting the joints, and alterations in gut microbiota are believed to play a key role in its development. Altered gut bacteria can lead to increased immune system activation and joint inflammation, worsening RA symptoms.111
- Osteoarthritis (OA): Systemic inflammation linked to dysbiosis can contribute to cartilage degradation, which leads to joint pain, disability, and reduced quality of life with OA.112
- Fibromyalgia: Fibromyalgia is a chronic condition characterized by widespread musculoskeletal pain, fatigue, and tenderness in various body parts. Recent research links fibromyalgia to gut health, with evidence suggesting that dysbiosis and gut inflammation may exacerbate symptoms by increasing systemic inflammation and affecting pain sensitivity.113
Cancer
Cancer is a complex group of diseases characterized by uncontrolled cell growth that may spread to other parts of the body. Risk factors include genetic predispositions, environmental exposures, and chronic inflammation that can be driven in part by dysbiosis and intestinal permeability.
Impact of gut health on cancer:
- Chronic inflammation: Persistent inflammation from leaky gut can initiate and promote cancer development by causing DNA damage and encouraging tumor growth.114
- Immune dysregulation: A disrupted gut barrier and altered microbiome can impair immune responses, reducing the body’s ability to detect and destroy cancer cells.115
- Cancer therapy effectiveness: Dysbiosis may affect the way the body responds to chemotherapy and immunotherapy, potentially altering the effectiveness of these treatments.116
Root Cause Approach to Achieving Optimal Gut Health
Healing the gut involves several key strategies to address and repair gut dysfunction, including dietary changes, targeted supplementation, and lifestyle adjustments. Following a structured approach using the 5R program can help restore a healthy gut microbiome, reduce inflammation, and improve overall bodily function.
5R program
The 5R program is a systematic approach to gut healing:117
- Remove: The first step is to eliminate factors that negatively affect gut health, such as:
- Harmful foods: processed foods, added sugars, and potentially triggering foods such as dairy and gluten.
- Toxins and allergens: Environmental toxins, common food allergens.
- Gut imbalances: Address infections or bacterial imbalances (dysbiosis) through targeted treatments.49 See specific protocols in the following section for examples.
- Replace: Next, support digestion by adding missing components (see Supplements 101).
- Digestive enzymes: Aid in nutrient breakdown and absorption.118
- Hydrochloric acid (HCl): HCl can aid in protein digestion if stomach acid levels are low.119
- Bile salts: Adequate bile salts are necessary for digesting fats120 and are stimulated by adequate dietary healthy fats and fiber, hydration, bitter foods like dandelion and cruciferous vegetables, and bile supplements.121
- Reinoculate: Reintroduce beneficial bacteria to the gut and support their balance.
- Probiotics: Beneficial microbes found in supplements with a daily dose typically ranging from 1–10 billion CFUs or fermented foods like kimchi and miso122 that help restore a healthy balance of gut microbiota, improving digestion and supporting immune function.123
- Strains such as Lactobacillus acidophilus, Bifidobacterium bifidum, Lactobacillus rhamnosus GG, and Bifidobacterium lactis BB-12 improve gut health and immune function.124
- Prebiotics: Non-digestible fibers that act as food for these good bacteria, encouraging their growth and keeping the gut ecosystem thriving.125
- Foods like bananas, onions, garlic, and leeks contain inulin and fructooligosaccharides (FOS), nourishing beneficial bacteria.125
- Supplements containing these fibers, 5–10 grams daily to nourish and support beneficial bacteria.
- Polyphenols: Polyphenols in berries (such as blueberries and strawberries), green tea, apples, onions, and dark chocolate126 have antioxidant and anti-inflammatory properties that support the microbiome by reducing oxidative stress and inflammation.127
- Polyphenols act as prebiotics, nourishing beneficial gut bacteria like Akkermansia muciniphila, which enhances metabolic health and strengthens the gut barrier.127
- Catechins in green tea help increase Akkermansia muciniphila levels, supporting gut lining integrity and metabolic health.128
- Specific polyphenols, such as quercetin in onions and apples, promote the growth of beneficial bacteria like Bifidobacteriaand Lactobacilli, which are essential for gut stability and immune function.129
- Probiotics: Beneficial microbes found in supplements with a daily dose typically ranging from 1–10 billion CFUs or fermented foods like kimchi and miso122 that help restore a healthy balance of gut microbiota, improving digestion and supporting immune function.123
- Repair: Heal the gut lining.
- Whole foods diet: A diet rich in vitamins and minerals from fruits, vegetables, lean proteins, and healthy fats supports tissue repair130 while avoiding processed foods, excessive sugar, alcohol, gluten, and dairy, which can irritate the gut and contribute to dysbiosis (see Nutrition 101).
- Nutrients: L-glutamine, zinc, and omega-3 fatty acids support repair and reduce inflammation.49
- Herbal remedies: Aloe vera and slippery elm have anti-inflammatory properties.131
- Rebalance: Finally, restore overall balance by managing stress, getting adequate sleep, and maintaining a healthy lifestyle.
- Stress management: Mindfulness and regular exercise are essential for long-term gut health and overall well-being132 (see Mental Health 101 and Stress Management 101).
- Sleep: Consistent sleep routine supports overall well-being (see Sleep 101).
- Exercise: Regular physical activity can stimulate bowel motility and help balance inflammation133 (see Exercise 101).
5R protocols for common gut health issues
The 5R approach focuses on removing harmful factors, replacing what’s missing, reinoculating the gut with beneficial bacteria, repairing the gut lining, and rebalancing lifestyle factors to help heal various gut issues. Each protocol integrates diagnosis, treatment options, and specific supplements that can support gut health (see Supplements 101).
Irritable bowel syndrome with constipation (IBS-C)
IBS-C is characterized by persistent constipation, abdominal discomfort, and bloating.
Diagnosis
Diagnosis often involves ruling out other conditions through medical history, symptom evaluation, and sometimes stool tests or imaging.134
- Rule out other conditions: Exclude conditions with similar symptoms, such as inflammatory bowel disease (IBD), celiac disease, thyroid disorders, and gastrointestinal infections using tests like complete blood count, comprehensive metabolic panel, thyroid panels, and stool cultures.135
- Rome IV Criteria for IBS-C: Confirm IBS-C diagnosis with recurrent abdominal pain at least once per week over the past three months, with constipation predominant (hard or lumpy stools >25% of the time and loose stools <25% of the time).136
- Specialized testing:
- Vinculin & CdtB antibodies: Elevated levels of these antibodies can indicate post-infectious IBS.137
- Complete blood count (CBC): reveal signs of past infections that might lead to post-infectious IBS.
- Breath testing: A lactulose breath test detects hydrogen and methane levels to diagnose SIBO, often associated with IBS-C due to high methane production.138
- Comprehensive stool test: Identifies dysbiosis and imbalances in gut bacteria or fungal overgrowth.139
- Food sensitivity testing: A food sensitivity panel can pinpoint dietary triggers that exacerbate IBS-C symptoms.140
- Cortisol: Salivary cortisol testing maps cortisol levels to assess stress responses, which are known to impact IBS-C.141
Remove
- Elimination diet: Remove common triggers like gluten, dairy, and high-FODMAP foods for 6–8 weeks to identify and remove food triggers, which should be followed by gut-healing therapies and gradual reintroduction of foods (see Nutrition 101).
- Low-FODMAP diet: Reducing foods high in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) can improve IBS-C symptoms. Key examples include wheat, onions (high in fructans), dairy (lactose), apples and pears (fructose), and sorbitol (found in sugar-free products). This diet helps decrease bloating and abdominal pain and also improves bowel function.142
- Dietary adjustments: Reduce intake of processed foods and increase fiber intake (gradually) to avoid bloating.
- Assess for gut dysbiosis or small intestinal fungal overgrowth (SIFO) through stool testing.
- Antimicrobials: If methane-dominant SIBO is present, consider treatments such as rifaximin with neomycin or herbal options like allicin.
- Antibiotics: A trial of metronidazole or neomycin may be prescribed for IBS-C.143
Replace
- Hydration: Ensure adequate fluid intake to aid digestion and stool passage.142
- Digestive enzymes: Use enzymes, particularly those containing lipase and protease, to aid in digestion.
- Ginger: A powerful, natural prokinetic that aids in gastric emptying and facilitates the smooth movement of intestinal contents.144 Dosage of 500–1,000 mg of ginger at night before bed can support these processes.
- Magnesium citrate: Introduce magnesium citrate to help promote bowel movements and ease constipation; 200–400 mg daily.
Reinoculate
- Probiotics: Strains like Bifidobacterium and Lactobacillus support gut flora;145 follow recommended dosages.
Repair
- Heal the gut lining with:
- L-Glutamine: Supports gut lining repair and reduces intestinal permeability, aiding overall gut health. Dosage of 5–10 grams daily.146
- Zinc: Enhances mucosal barrier function. Dosage of 15–30 mg daily.147
- Slippery elm: Provides a protective layer to the gut lining. Dosage of 400–800 mg daily.131
- Omega-3 fatty acids: Reduce inflammation and support gut health. Dosage of 1–3 grams daily.148
Rebalance
- Exercise: Regular physical activity can stimulate bowel movements (Hamaguchi, 2020)133 (see Exercise 101).
- Stress management: Practices such as yoga, meditation, or deep breathing exercises149 (see Mental Health 101 and Stress Management 101).
Medications
- Laxatives: In some cases, osmotic laxatives like polyethylene glycol150 may be recommended if necessary. Often used short-term. Overuse can lead to dependence and may worsen symptoms.
- GI motility agents: Lubiprostone or linaclotide may be prescribed to improve bowel movements by increasing intestinal fluid secretion and motility. Effective for some patients but may cause gastrointestinal side effects such as diarrhea and abdominal pain.150
- Antispasmodics (e.g., hyoscine, dicyclomine): Relieve abdominal pain and cramping by relaxing intestinal smooth muscle. Primarily used for symptom relief. Long-term use may not address the underlying cause.151
- Tricyclic antidepressants (e.g., amitriptyline, nortriptyline): Alleviate abdominal pain and improve bowel symptoms through their analgesic and anticholinergic properties. Can be effective for pain but may have side effects like dry mouth and drowsiness; do not target root causes of IBS-C.152
Irritable bowel syndrome with diarrhea (IBS-D)
IBS-D is characterized by frequent diarrhea, abdominal pain, and urgency.
Diagnosis
Diagnosing IBS-D involves a multi-step process to ensure an accurate diagnosis and identify root causes and triggers.134
- Rule out other conditions: IBS-D symptoms overlap with various conditions like inflammatory bowel disease (IBD), celiac disease, and infections. To exclude these, tests such as complete blood count, comprehensive metabolic panel, and stool cultures are conducted.135
- Rome IV Criteria: Confirm diagnosis based on Rome IV criteria—recurrent abdominal pain at least once a week over three months, with changes in stool frequency and consistency, predominated by diarrhea.136
- Specialized testing: Conduct additional tests such as:
- Vinculin & CdtB antibodies: Elevated levels indicate post-infectious IBS.137
- SIBO breath test: Elevated hydrogen levels in breath samples can indicate small intestinal bacterial overgrowth, which is commonly associated with IBS-D.153
- Comprehensive stool analysis: Helps identify dysbiosis, such as imbalances in gut bacteria and fungal overgrowth.139 It also assesses for bile acid diarrhea and pancreatic insufficiency.154
- Food sensitivity testing: Identifies specific food triggers that may worsen IBS-D symptoms, allowing for more personalized dietary adjustments.155
Remove
- Trigger elimination:
- Elimination diet: Remove common triggers like gluten, dairy, and high-FODMAP foods to reduce symptoms.156
- Low-FODMAP diet: Avoid foods high in fermentable carbohydrates, such as wheat, onions, dairy, apples, and sorbitol-containing products, to alleviate bloating and abdominal pain and improve bowel function 157 (see Nutrition 101).
Replace
- Maintain hydration to replace lost fluids from diarrhea.
- Support digestion with digestive enzymes if pancreatic insufficiency is detected.154
Reinoculate
- Probiotics: Restore gut flora with probiotics, focusing on Lactobacillus and Bifidobacterium strains to balance the microbiome.145
- Psyllium husk: Provides bulk to stool by adding soluble fiber and aids in bowel regulation;158 take as directed.
Repair
- Heal the gut lining using:
- L-glutamine: Helps repair the gut lining and reduce inflammation. Dosage of 5–10 grams daily.146
- Omega-3 fatty acids: Help reduce inflammation and support gut health. Dosage of 1–3 grams daily.148
- Quercetin: Provides antioxidant protection and supports gut integrity. Dosage of 500–1,000 mg daily.
- Further rebalance inflammation and soothe the digestive tract with:
- Curcumin: Reduces gut inflammation and oxidative stress. Dosage of 500–1,000 mg daily.159
- Peppermint oil: Soothes digestive tract muscles, reducing pain, bloating, and urgency.160
Rebalance
- Stress management: Implement techniques like meditation, yoga, and deep breathing exercises to manage stress, which can exacerbate IBS-D symptoms 161(see Mental Health 101 and Stress Management 101).
- Regular exercise: Engage in moderate physical activity to improve gut motility and overall digestive health 162(see Exercise 101).
Medications
- Antidiarrheals: Medications like loperamide are sometimes used as needed.163
- Prescriptions: Eluxadoline is another medication that works by targeting opioid receptors in the gut to reduce bowel motility and pain.163
Small Intestinal Bacterial Overgrowth (SIBO)
Diagnosis
SIBO is diagnosed through breath tests that measure hydrogen and methane levels produced by bacteria in the small intestine after ingesting a sugar solution to assess bacterial fermentation and overgrowth.153 Additionally, clinical symptoms and patient history are considered to support the diagnosis.164 Treatment is personalized and targeted toward the type of imbalances found with testing and symptoms.
- Breath testing: The breath test is the most commonly used method for diagnosing SIBO. After a one-day preparatory diet, patients consume a glucose- or lactulose-containing solution. The breath is then analyzed for hydrogen, methane, and hydrogen sulfide gasses to identify SIBO and its subtypes:153
- Hydrogen-dominant SIBO: Diagnosed if hydrogen levels increase by at least 20 ppm from baseline within the first 90 minutes.
- Methane-predominant SIBO (IMO): Diagnosed if methane levels are 10 ppm or higher at any point during the test.
- Hydrogen sulfide-dominant SIBO: Diagnosed if hydrogen sulfide levels reach at least 3 ppm at any time during the test.
Laboratory studies may also be used to investigate the root causes of SIBO:
- Vinculin & CdtB antibodies: Elevated levels of these antibodies can indicate post-infectious IBS, which is linked to SIBO.137
- Thyroid: Hypothyroidism can slow digestion and exacerbate symptoms.165 A comprehensive thyroid assessment checks for thyroid hormone imbalances and autoimmune conditions.
- Hemoglobin A1c (HbA1c): Measures average blood sugar levels over three months, helping to identify diabetes-related nerve damage that can affect intestinal motility.166
- Cortisol testing: Chronic stress can disrupt gastrointestinal function.167 Salivary cortisol tests measure cortisol patterns to assess stress impacts on digestion.
- Comprehensive stool analysis: Helps identify dysbiosis, such as imbalances in gut bacteria and fungal overgrowth.139
- Imaging: In some cases, imaging techniques like endoscopy, colonoscopy, or antroduodenal manometry may be necessary to rule out structural issues or inflammatory bowel disorders.168
Remove
Targeted removal strategies address specific types of dysbiosis (or microbial imbalance):
- Methane (CH4) dysbiosis: For excessive methane production, which is often associated with constipation, the removal step might involve antibiotics or herbal antimicrobials like oregano oil or berberine169 to target methane-producing bacteria.170
- Hydrogen (H2) dysbiosis: High hydrogen levels, often causing diarrhea, may require similar treatments to target hydrogen-producing bacteria, such as antibiotics like rifaximin or herbal remedies like garlic.170
- Sulfide (H2S) dysbiosis: Sulfide-producing bacteria171 that produce hydrogen sulfide, aka rotten egg gas, can be managed with targeted medications or herbs like cilantro, which help detoxify and reduce sulfide levels associated with certain types of bacterial overgrowth.
- Parasites and worms: For parasitic infections, treatments include antiparasitic medications such as albendazole172 or herbal antiparasitics like black walnut173 and wormwood.174
- Yeast: Candida and other yeast infections may require antifungal medications like fluconazole175 or natural antifungals like caprylic acid176 and garlic.177
Herbal antimicrobials can be used to target specific patterns of overgrowth170 and inflammation in the gut. Commonly used herbal antimicrobials for SIBO include:
- Berberine: A compound found in herbs like goldenseal, berberine has strong antimicrobial and anti-inflammatory effects, making it effective in reducing SIBO symptoms by targeting a wide range of pathogenic bacteria.178 Dosage of 500 mg twice daily.
- Oregano oil: Used for its potent antimicrobial properties, particularly against gram-positive bacteria and fungi, which helps reduce bacterial overgrowth in the small intestine.170 A typical dose is 100–200 mg of oregano oil, taken two to three times daily with meals, to effectively target and manage SIBO.
- Garlic (Allium sativum): Known for its broad-spectrum antibacterial and antifungal effects, garlic helps target a variety of gut pathogens and supports overall digestive health.179 A common dose is 600–1,200 mg of garlic extract daily, divided into two to three doses with meals, to effectively manage SIBO and enhance gut health.
- Neem leaf: Neem helps reduce bacterial overgrowth and supports gastrointestinal health by targeting harmful microbes.
- Wormwood: Provides anti-inflammatory and antimicrobial benefits that may aid in symptom relief and support remission. Typically taken in doses of 200–500 mg, two to three times per day, it contains compounds that may inhibit microbial growth and reduce gut inflammation, but it should be used for short periods under professional guidance.180
Antibiotics may be used in combination with herbal options or as an alternative:
- Antibiotics: Rifaximin is commonly prescribed for hydrogen-dominant and hydrogen sulfide-dominant SIBO, with alternatives like amoxicillin-clavulanic acid and metronidazole also used. Treatment typically involves a two-week course, though multiple courses may be necessary.169 Neomycin may be added for methane SIBO. Bactrim DS may be added for sulfide SIBO.
Dietary approaches can also help with removing triggers and food for the overgrown bacteria:
- Low-FODMAP diet: A low-FODMAP diet, which reduces fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, can significantly improve symptoms of bloating in SIBO by helping to reduce fermentable food for bacteria. Examples include foods high in fructans like wheat and onions, dairy products containing lactose, fruits high in fructose like apples and pears, and polyols such as sorbitol found in sugar-free products and certain fruits. This diet helps reduce bloating and abdominal pain while improving bowel function and giving insights into triggers to avoid.181
- Specific carbohydrate diet (SCD): This diet treats SIBO by eliminating fermentable carbohydrates that feed the overgrowth of bacteria in the small intestine, thereby reducing symptoms and promoting gut healing through a restrictive, low-residue diet.182 The SCD eliminates complex carbohydrates, sugars, grains, legumes, most dairy products, and processed foods to reduce bacterial fermentation and improve gut health. It includes easily digestible fruits, vegetables, fresh meats, fish, nuts, seeds, eggs, and certain fermented foods like homemade yogurt and aged cheeses.
- Elemental diet: Provides pre-digested, nutrient-rich formulas that are easily absorbed in the small intestine, minimizing the food available for bacterial fermentation. This diet effectively reduces bacterial overgrowth by giving the gut a few weeks’ break from digesting whole foods, allowing the reduction of symptoms and the restoration of gut balance. This diet provides predigested nutrients to starve bacteria while nourishing the patient. It’s highly effective but may not be suitable for everyone, especially those with diabetes.183
Replace
- Digestive enzymes: For those with low stomach acid (hypochlorhydria), digestive enzymes like betaine hydrochloric acid (HCl) can be taken with meals to supplement stomach acid levels. A betaine HCl challenge is often useful for determining the appropriate dosage for each meal.184
- Bitters: Digestive bitters are another option to naturally enhance the body’s own digestive enzyme production and improve intestinal blood flow. Foods like arugula, cacao, and radicchio, along with bitter herbs such as gentian, dandelion root, and chamomile, can be particularly supportive when consumed 15–20 minutes before meals.185
- Ginger: A powerful, natural prokinetic that aids in gastric emptying and facilitates the smooth movement of intestinal contents.144 Dosage of 500–1,000 mg of ginger at night before bed can support these processes.
Reinoculate
- Probiotics: Specific strains like Saccharomyces boulardii and Lactobacillus species can reduce inflammation, inhibit pathogenic bacteria, and support overall gut health.186
Repair
Heal the gut lining and reduce inflammation with:
- L-glutamine: Aids in gut lining repair and reduces permeability. Dosage of 5–10 grams daily.146
- Curcumin: Reduces inflammation in the gut. Dosage of 500–1,000 mg daily.159
- Aloe vera: Soothes and repairs the gut lining. Dosage of 100–300 mg daily.187
- Quercetin: Supports gut integrity and reduces inflammation.188 Dosage of 500–1,000 mg daily.
Rebalance
- Stress management: Practice stress reduction techniques such as mindfulness, yoga, or deep breathing exercises to support overall gut health (See Mental Health 101 and Stress Management 101).
- Regular exercise: Engage in regular physical activity to support digestion and overall health. Exercise can improve gut motility and reduce symptoms (see Exercise 101).
- Adequate sleep: Ensure consistent, restful sleep to support digestive health and overall well-being (see Sleep 101).
Small Intestinal Fungal Overgrowth (SIFO)
SIFO causes digestive issues such as bloating and abdominal pain, systemic symptoms like fatigue, skin problems, and increased food sensitivities, and it is often accompanied by mental health symptoms like brain fog.
Diagnosis
Diagnosis involves testing for fungal overgrowth in the small intestine, often through a bowel aspirate to remove and test contents of the small intestine,189 stool tests, or breath tests to rule out bacterial overgrowth that can cause similar symptoms.
Remove
- Anti-candida diet: This diet focuses on consuming non-starchy vegetables, low-sugar fruits, gluten-free grains, limited dairy, and fermented foods, avoiding sugars, fruit juice, white bread and pasta, and baked goods to reduce yeast overgrowth and restore gut balance by minimizing sugar and inflammation.190
- Low-FODMAP diet: This approach restricts short-chain carbohydrates that can be hard to digest and may contribute to yeast and bacterial overgrowth, with an emphasis on avoiding foods like legumes, corn, and cruciferous vegetables, and often includes a gluten-free or grain-free component to alleviate symptoms that overlap with SIFO and SIBO.181
- Elemental diet: This strategy uses a liquid formula containing pre-digested proteins, fats, and carbohydrates along with essential nutrients to provide complete nutrition while excluding fiber, aiming to starve bacteria in the small intestine for 2–3 weeks while ensuring adequate nourishment.183
- Herbal antimicrobials: Candida and other yeast infections may require natural antifungals like caprylic acid176 and garlic177 to reduce the overgrowth.
- Antifungals: Antifungal medications like fluconazole, itraconazole, or nystatin175 may be required to reduce the overgrowth of Candida.
Replace
Dysmotility and low stomach acid are two key, modifiable risk factors for SIFO, so targeted lifestyle changes and supplements can play a critical role in enhancing gastrointestinal motility and boosting digestive enzyme production.
- Digestive enzymes: For those with low stomach acid (hypochlorhydria), digestive enzymes like betaine hydrochloric acid (HCl) can be taken with meals to supplement stomach acid levels. A betaine HCl challenge is often useful for determining the appropriate dosage for each meal.184
- Bitters: Digestive bitters are another option to naturally enhance the body’s own digestive enzyme production and improve intestinal blood flow. Foods like arugula, cacao, and radicchio, along with bitter herbs such as gentian, dandelion root, and chamomile, can be particularly supportive when consumed 15–20 minutes before meals.185
- Ginger: A powerful, natural prokinetic that aids in gastric emptying and facilitates the smooth movement of intestinal contents.144 Dosage of 500–1,000 mg of ginger at night before bed can support these processes.
- Mindful eating: Paying attention to the act of eating and eating in a peaceful setting helps to engage the parasympathetic nervous system, which promotes healthy digestive enzyme secretion and effective intestinal contractions necessary for optimal digestion, nutrient absorption, and waste elimination. To foster a mindful eating environment, set aside dedicated time for meals, minimize distractions, and fully engage the senses in the eating process.191
Reinoculate
- Probiotics: Probiotic strains like Saccharomyces boulardii, Lactobacillus rhamnosus, Lactobacillus acidophilus, and Bifidobacterium bifidum help reduce candida overgrowth in SIFO by competing with candida, lowering gut pH, and supporting a balanced gut microbiome. These probiotics create an environment that discourages fungal proliferation and promotes gut health.192
- Rebalance the gut microbiome: Adopting a Mediterranean-style diet rich in fruits, vegetables, legumes, and fish, alongside probiotic and prebiotic foods, helps support gut health and balances the microbiome by reducing inflammation and promoting beneficial bacteria (see Nutrition 101).
Repair
Heal the gut lining and reduce inflammation with:
- L-glutamine: Supports gut repair and reduces permeability. Dosage of 5–10 grams daily.146
- Curcumin: Provides anti-inflammatory and antioxidant benefits. Dosage of 500–1,000 mg daily.159
- Omega-3 fatty acids: Reduces gut inflammation. Dosage of 1–3 grams daily.148
- Aloe vera: Soothes the digestive tract. Dosage of 100–300 mg daily.187
- Vitamin D: Supports immune function and helps regulate the gut microbiome, potentially reducing fungal overgrowth and promoting gut healing.193 Dosage of 2,000 IU daily.
- Zinc carnosine: Enhances mucosal integrity and repairs gut lining, aiding in the recovery from fungal overgrowth and reducing inflammation in the digestive tract.194 Dosage of 50 mg twice daily.
Rebalance
- Stress management: Practice stress reduction techniques such as mindfulness, yoga, or deep breathing exercises to support overall gut health (see Mental Health 101 and Stress Management 101).
- Regular exercise: Engage in regular physical activity to support digestion and overall health. Exercise can improve gut motility and reduce symptoms (see Exercise 101).
- Adequate sleep: Ensure consistent, restful sleep to support digestive health and overall well-being (see Sleep 101).
Gastroesophageal Reflux Disease (GERD)
Gastroesophageal reflux disease (GERD) is a chronic condition where stomach acid frequently leaks into the esophagus, causing symptoms such as heartburn, regurgitation, and discomfort.
Diagnosis
GERD is typically diagnosed through a combination of:
- Clinical symptoms.
- Response to an eight-week trial of proton pump inhibitors (PPIs).
- Endoscopic evaluation when needed to assess esophageal inflammation.
- If endoscopy results are normal but symptoms persist, reflux monitoring over 24 hours can confirm the diagnosis.
- Comprehensive gut testing, including stool analysis and SIBO breath testing, may be used to assess underlying factors contributing to GERD symptoms.195
Remove
- Dietary adjustments: Avoid trigger foods like spicy or fatty foods, caffeine, and alcohol. Eat smaller, more frequent meals, and avoid eating within 2–3 hours before bedtime196 (see Nutrition 101).
- Antimicrobials: To address any bacterial dysbiosis contributing to excess gas production and intra-abdominal pressure. Herbal options to address dysbiosis include:
- Berberine: 500–1,000 mg, three times daily.197
- Oregano oil: 50 mg, three times daily.198
- Neem leaf: 600 mg, three times daily.199
- Lifestyle changes: Elevate the head of the bed and avoid lying down immediately after eating.196
- Maintain a healthy weight: Reducing excess weight, especially reducing central abdominal fat, to decrease pressure on the lower esophageal sphincter (LES), can help treat GERD196 (see Weight Management 101).
- Avoid tobacco: Quit smoking and avoid tobacco products.196
Replace
- Digestive enzymes: For those with low stomach acid (hypochlorhydria), digestive enzymes like betaine hydrochloric acid (HCl) can be taken with meals to supplement stomach acid levels. A betaine HCl challenge is often useful for determining the appropriate dosage for each meal.184
Reinoculate
- Probiotics (Lactobacillus & Bifidobacterium): Supports gut flora balance and helps normalize gastric acid levels;200 up to 46 billion CFU daily.
Repair
Heal the gut lining and reduce inflammation with:
- L-glutamine: Supports gut lining and helps repair any damage. Dosage of 5–10 grams daily.146
- Slippery elm: Coats and soothes the esophageal lining. Dosage of 400–800 mg daily.131
- Omega-3 fatty acids: Helps reduce inflammation. Dosage of 1–3 grams daily.148
- Aloe vera: Soothes the digestive tract and supports mucosal healing. Dosage of 100–300 mg daily.187
- Deglycyrrhizinated licorice (DGL): Soothes and heals the esophagus. Dosage of 760 mg, three times daily before meals.201
- Zinc carnosine: Has gastrointestinal protective effects, particularly in managing conditions like gastroesophageal reflux disease (GERD) or reflux. It has anti-inflammatory and antioxidant effects, promotes gastric cell regeneration, and regulates gastric acid secretion. The typical dosage of zinc carnosine for gastrointestinal health and the management of reflux symptoms is 75 mg to 150 mg per day, usually divided into two doses.
Rebalance
- Manage stress: Managing stress is also important, as it can influence digestive health and GERD symptoms202 (see Mental Health 101 and Stress Management 101)
Medications
- Proton pump inhibitors (PPIs): PPIs are often prescribed for GERD to promote mucosal healing and reduce symptoms. Common options include esomeprazole and omeprazole. Typically, a once-daily dose for eight weeks is recommended. For those with more severe or extraesophageal symptoms, a twice-daily regimen may be used. After improvement, the goal is to taper off PPIs, switch to on-demand use, or replace with a milder H2RA medication, using the lowest effective dose to maintain symptom control.203
Inflammatory Bowel Disease (IBD)
IBD includes conditions like Crohn’s disease and ulcerative colitis.
Diagnosis
To diagnose IBD, a combination of blood work, stool tests, and specialized screenings is used to assess the severity and underlying causes of the disease.
- Blood tests like CBC, CMP, hs-CRP, and ESR help evaluate anemia, malnutrition, inflammation, and organ function.
- Comprehensive stool tests, including leukocytes, calprotectin, and lactoferrin identify inflammation and immune activity in the gut.
- ASCA and pANCA help differentiate between Crohn’s and UC.
- Food sensitivity tests and SIBO breath tests can uncover triggers of inflammation.
- Micronutrient testing and health screenings, such as DEXA scans and colonoscopies, monitor nutrient deficiencies and the risk of osteoporosis or colon cancer in IBD patients.204
Remove
- Diet adjustments during an IBD flare: Avoid foods that are inflammatory or hard to digest, such as high-fiber foods, lactose, refined sugars, and gluten. Opt for a low-residue diet or an elemental diet to reduce gastrointestinal stress and ensure nutritional needs are met.205
- Avoid tobacco: Avoiding tobacco, including quitting smoking if a smoker and avoiding secondhand smoke, is important for managing IBD, as tobacco use can worsen symptoms and increase disease severity, especially in Crohn’s disease.206
Replace
- Digestive enzymes: Individuals with IBD may have impaired digestion and enzyme deficiencies. Supplement with digestive enzymes to support the breakdown of proteins, fats, and carbohydrates. Enzymes like protease, lipase, and amylase can be used to enhance nutrient absorption and to reduce symptoms.207
- Hydrochloric acid: If low stomach acid is suspected, betaine hydrochloric acid (HCl) can be taken with meals to support digestion and improve nutrient absorption. A betaine HCl challenge test may help determine the appropriate dosage.184
Reinoculate
- Probiotics: Strains like Saccharomyces boulardii and specific Lactobacillus and Bifidobacterium strains.208
Repair
Heal the digestive tract and reduce inflammation with:
- Curcumin: The active compound in turmeric, curcumin, reduces inflammation and can enhance the effects of other therapies.209 Dosage of 500–1,000 mg daily.159
- L-glutamine: Aids in gut lining repair and reduces permeability. Dosage of 5–10 grams daily.146
- Omega-3 fatty acids: Helps reduce inflammation. Dosage of 1–3 grams daily.148
- Zinc: Supports gut barrier integrity. Dosage of 15–30 mg daily.147
- Vitamin D: Supports immune function.210 Dosage of 1,000–2,000 IU daily.
- Boswellia serrata: Reduces inflammation by inhibiting inflammatory mediators, comparable in effect to traditional anti-inflammatory drugs.211,212 To reduce inflammation, dosage of 300–500 mg of boswellia extract, typically standardized to contain 60-65% boswellic acids, is usually taken two to three times daily.213
- Wormwood: Offers anti-inflammatory and antimicrobial benefits, potentially supporting remission and symptom relief. Dosage typically ranges from 200–500 mg, taken two to three times per day.180 This should only be used for brief periods of time and under the direction of a healthcare professional.
- Aloe vera: Provides anti-inflammatory benefits that may alleviate symptoms of ulcerative colitis.187 Generally, doses start at 1–2 tablespoons (15–30 mL) of aloe vera juice, taken one to two times daily, typically before meals. Aloe vera juice should be pure and free from added sugars or artificial ingredients.214
- Peppermint oil: Soothes digestive tract muscles, reducing pain and bloating.160 Doses range from 180–200 mg of enteric-coated peppermint oil capsules, taken two to three times daily before meals. This enteric coating helps ensure that the oil is released in the intestines rather than the stomach, which maximizes its effectiveness for gastrointestinal issues.215
Rebalance
- Long-term dietary approach: Focus on a balanced diet rich in fiber and omega-3 fatty acids to prevent malnutrition and relapse. Continue to avoid specific food sensitivities like wheat and dairy 216(see Nutrition 101).
- Manage stress: Effective stress management is essential for IBD patients, as high stress levels can trigger flare-ups and exacerbate gastrointestinal symptoms 217(see Mental Health 101 and Stress Management 101).
Medications:
- Anti-inflammatory drugs: 5-ASA compounds and corticosteroids.218
- Immunosuppressants: Azathioprine or methotrexate.218
- Biologics: Infliximab, adalimumab for severe cases.218
Dysbiosis
Dysbiosis refers to an imbalance in the gut microbiome, where harmful bacteria or other microbes outnumber beneficial ones due to a decline in beneficial bacteria, overgrowth of potentially harmful bacteria, and/or loss of overall bacterial diversity.48
Diagnosis
- Clinical assessment: Evaluate symptoms such as digestive discomfort, bloating, and changes in bowel habits.
- Laboratory tests: Perform stool analysis to identify microbial imbalances and assess overall gut microbiome diversity.
- Breath tests: Utilize tests for hydrogen and methane to detect bacterial overgrowth or fermentation issues.153 See SIBO and SIFO protocols.
Remove
- Dietary triggers: Avoid foods that exacerbate dysbiosis, including high-sugar and high-fat foods, which can fuel harmful microbial overgrowth.219
- Pathogen management: Use antimicrobial agents as necessary to address pathogenic bacteria or yeast. Options include herbal antimicrobials such as oregano oil, neem, wormwood, and garlic. See SIBO and SIFO protocols.
- Berberine: 500-1,000 mg, three times daily.197
- Oregano oil: 50 mg, three times daily.198
- Neem leaf: 600 mg, three times daily.199
- Garlic (Allium sativum): Broad-spectrum antibacterial and antifungal effects.179 Dosage 600–1,200 mg of garlic extract daily, divided into two to three doses with meals.
- Wormwood: Anti-inflammatory and antimicrobial; 200–500 mg, two to three times per day only under guidance.180
Replace
- Digestive enzymes: Supplement with enzymes like protease, lipase, and amylase to aid digestion and reduce microbial fermentation.
- Hydrochloric acid (HCl): If low stomach acid is present, use betaine HCl to support gastric acid levels and improve digestion.184
Reinoculate
- Probiotics: Introduce beneficial bacteria, such as Lactobacillus and Bifidobacterium, to improve gut balance and health.
- Prebiotics: Nourish beneficial bacteria with prebiotic fibers to support their growth and function.
- Polyphenols: Consume polyphenol-rich foods, which act as prebiotics, stimulate beneficial gut bacteria, and help reduce inflammation.127
Repair
- L-glutamine: Supplement with 5–10 grams daily to support gut lining repair and reduce permeability.146
- Curcumin: Use 500–1,000 mg daily for its anti-inflammatory properties to aid gut healing .159
- Omega-3 fatty acids: Taking 1–3 grams daily can help reduce inflammation and support gut health.148
Rebalance
- Dietary strategies: Emphasize whole foods, fiber-rich fruits and vegetables, and anti-inflammatory foods.220
- Lifestyle changes: Manage stress, prioritize sleep, and engage in regular physical activity to support overall health and reduce gut-related issues 221(see Mental Health 101 and Stress Management 101).
Leaky Gut
Leaky gut syndrome is characterized by increased intestinal permeability. This condition arises when the tight junctions in the gut lining, which normally control what passes through the intestinal wall, become loosened.50
Diagnosis
- Symptom assessment: Evaluate gastrointestinal symptoms such as bloating, gas, diarrhea, constipation, and abdominal pain as well as systemic symptoms like fatigue, headaches, and skin issues.
- Intestinal permeability testing: Utilize tests like the lactulose/mannitol test to measure the absorption of these sugars and assess the permeability of the gut lining. An increase in lactulose relative to mannitol indicates leaky gut.222
- Stool analysis: Perform comprehensive stool tests to assess gut flora balance, detect potential pathogens, and identify markers of inflammation or dysbiosis. This helps to evaluate the health of the gut microbiome.
- Endoscopy and biopsy (if needed): For persistent symptoms or when other tests are inconclusive, an endoscopy with biopsy may be conducted to examine the gut lining directly and rule out other conditions.
- Food sensitivity testing: Identify potential food sensitivities or allergies that might contribute to inflammation and gut permeability. This can guide dietary modifications to reduce symptoms.
Remove
- Identify and eliminate trigger foods: Remove foods that may cause inflammation or sensitivity reactions in the gut, such as wheat, dairy, peanuts, soy, eggs, corn, and processed foods.
- Address gut infections: Test for and treat infections such as bacterial overgrowth, parasites, or fungal infections using prescription medications or antimicrobial herbs like berberine, oregano, neem, and garlic. See SIBO and SIFO protocols.
- Reduce toxin exposure: Limit contact with environmental toxins by avoiding cigarette smoke, choosing organic produce, drinking filtered water, and using air purifiers.
- Manage stress: Practice stress-reducing techniques such as meditation, deep breathing exercises, yoga, or mindfulness to support overall gut health.132
Replace
- Digestive enzymes: Supplement with digestive enzymes to enhance the breakdown of proteins, fats, and carbohydrates. This helps improve digestion and absorption, reducing gut inflammation.
- Hydrochloric acid: Consider adding hydrochloric acid (HCl) supplements if low stomach acid is detected to improve protein digestion and support overall gut health.184
- Nutrient replacement: To target any deficiencies due to malabsorption or restrictive diets.
Reinoculate
- Probiotics: Strains such as Lactobacillus rhamnosus and Bifidobacterium lactis have been shown to help restore gut barrier function and reduce intestinal permeability. Research indicates that these probiotics can enhance gut health by reducing inflammation and promoting the repair of the gut lining.223
- Prebiotics: Prebiotic fibers like inulin and fructooligosaccharides (FOS) support the growth of beneficial gut bacteria, which can enhance gut barrier function and reduce inflammation. Studies have demonstrated that prebiotics can improve symptoms of leaky gut by fostering a healthier microbiome and supporting mucosal repair.224
- Short-chain fatty acids (SCFAs): Acetate, propionate, and butyrate, produced by the fermentation of dietary fibers, help maintain gut barrier function, reduce inflammation, and support overall gut health.50
- Polyphenols: Compounds such as curcumin and resveratrol have anti-inflammatory and antioxidant properties that help protect the gut lining and reduce oxidative stress. Research shows that polyphenols can modulate gut microbiota, enhance gut barrier integrity, and mitigate inflammation associated with leaky gut.50
Repair
Heal the gut lining with:
- L-glutamine: Use L-glutamine to support gut lining repair and reduce intestinal permeability. Dosage: 5–10 grams daily.146
- Slippery elm: Incorporate slippery elm to coat and soothe the gut lining. Dosage: 400–800 mg daily.131
- Omega-3 fatty acids: Supplement with omega-3 fatty acids to reduce inflammation and support gut healing. Dosage: 1–3 grams daily.148
- Zinc carnosine: Supports mucosal repair and strengthens gut barrier function, aiding in the recovery from leaky gut.147
- Vitamin D: Plays a role in maintaining gut barrier function and modulating immune responses, contributing to reduced inflammation and improved gut health.210
- Marshmallow root: Similar to slippery elm, it provides mucilaginous compounds that help soothe and protect the gut lining.50
- Chamomile: Has anti-inflammatory properties that can help reduce gut inflammation and support mucosal healing.50
- Turmeric (curcumin): Contains curcumin, which has potent anti-inflammatory and antioxidant effects that promote gut health and repair.50
Rebalance
- Stress management: Implement stress reduction techniques such as mindfulness, meditation, and relaxation exercises to support gut health and reduce inflammation (see Mental Health 101 and Stress Management 101).
- Regular exercise: Engage in regular physical activity to promote overall health and support a balanced gut microbiome (see Exercise 101).
- Adequate sleep: Ensure sufficient, quality sleep to support the body’s repair processes and maintain healthy gut function (see Sleep 101).
Lifestyle changes
Lifestyle changes play an essential role in supporting gut health and overall well-being. Here are some key areas to focus on:
- Stress management: Chronic stress can disrupt the gut microbiome and exacerbate gut inflammation.132 Techniques such as mindfulness, meditation, and deep breathing exercises can help manage stress and promote gut health. Stress-reducing activities enhance gut microbiome diversity and improve gastrointestinal disease symptoms by lowering stress-induced inflammation and modulating the gut-brain axis, which regulates communication between the gut and brain.225 For example, in IBS, stress management techniques can alleviate symptoms such as abdominal pain and bloating by balancing gut microbiota and reducing inflammation through this gut-brain axis 226(see Mental Health 101 and Stress Management 101).
- Importance of sleep: Quality sleep is essential for maintaining a healthy gut. Poor sleep can negatively affect the gut microbiome, leading to dysbiosis and gastrointestinal issues.227 Aiming for 7–9 hours of uninterrupted sleep per night supports the body’s natural healing processes and maintains a balanced gut microbiota (see Sleep 101).
- Role of physical activity: Regular physical exercise contributes to a healthy gut by promoting beneficial bacterial growth and enhancing overall gut motility.221 Engaging in moderate exercise, such as brisk walking or cycling, for at least 150 minutes per week can help maintain a balanced microbiome and improve gut function (see Exercise 101).
Personalized approach to gut health
Addressing gut health effectively requires a personalized approach. Individualized assessment and treatment plans ensure that care is tailored to each person’s unique needs. Functional lab tests like those included in Function’s membership (or available as an add-on) provide detailed insights into gut health, identifying specific imbalances and deficiencies.
A root-cause medicine approach combines dietary adjustments, lifestyle changes, and targeted supplements to restore gut balance and promote overall well-being. By regularly monitoring and adjusting these plans based on progress, patients can achieve optimal health outcomes. This integrative approach ensures that each aspect of gut health is addressed, leading to sustainable improvements and a higher quality of life.
Function tests to assess gut health
Evaluating gut health with Function Health tests can pinpoint specific issues and guide personalized treatment plans.
- Adiponectin: Protein hormone involved in glucose regulation and fatty acid breakdown; levels can be influenced by gut health and linked to metabolic syndrome.
- Antinuclear antibodies (ANA): Detects autoimmune disorders linked to gut dysbiosis; positive results can indicate conditions like lupus (SLE) with gut-related symptoms.
- Celiac panel: Screens for celiac disease; identifies gluten intolerance, a common issue linked with gut health.
- Cortisol: Stress hormone; chronic stress impacts gut health, and cortisol levels can reflect this interaction.
- DHEA sulfate: Precursor to sex hormones and indicator of adrenal function; levels can be influenced by chronic stress and gut health.
- Ferritin: Indicates iron storage; levels can reflect gut absorption efficiency and inflammation.
- Folate: Vital for DNA synthesis and repair; gut health can affect folate absorption, impacting overall health.
- Food sensitivity testing: Identifies food sensitivities that can cause gut inflammation and symptoms.
- Glucose: Indicates blood sugar levels; imbalances can be linked to gut health and metabolic issues.
- Hemoglobin A1c (HbA1c): Measures long-term blood sugar control; high levels can be linked to metabolic disorders influenced by gut health.
- High-sensitivity C-reactive protein (hs-CRP): Measures inflammation; high levels indicate systemic inflammation often linked to gut health issues.
- Immunoglobulin A (IgA): Involved in immune function at mucosal surfaces like the gut; low levels may indicate compromised gut mucosal immunity and potential for gut inflammation or infections.
- Insulin: Indicates insulin levels and sensitivity; dysbiosis can affect insulin regulation, leading to metabolic issues.
- Leptin: Hormone that regulates hunger and energy balance; imbalances can be associated with gut health and obesity.
- Thyroglobulin antibodies (TgAb): Indicates autoimmune thyroid disease; autoimmune conditions related to gut health issues.
- Thyroid peroxidase (TPO) antibodies: Indicates autoimmune thyroid disease; autoimmune conditions like Hashimoto’s thyroiditis are often linked with gut health issues.
- Thyroid-stimulating hormone (TSH): Measures thyroid function; thyroid disorders are commonly associated with gut health problems.
- Vitamin B12: Essential for nerve function and red blood cell production; absorption can be impaired by gut issues, leading to deficiency.
- Vitamin D, 25-hydroxy: Essential for immune function and inflammation control; low levels are often linked to poor gut health and increased inflammation.
- White blood cell (WBC): General marker of immune response; elevated levels may signal infections or inflammation linked to gut health.
- Zinc, plasma or serum: Important for immune function and gut lining integrity; deficiency can impair gut barrier function and immunity.
Other tests to assess gut health
To understand the health of the gut microbiome, various tests can be conducted. One common method is a stool test, which analyzes the composition of the microorganisms in the gut. This test can provide information about the types and amounts of bacteria and other microbes present, helping to identify any imbalances or issues.228 Additionally, other tests, such as breath tests or endoscopies, can provide further insights into gut health and function. These tests are not part of a Function Health membership.
- Comprehensive stool analysis: Tests for pathogens, beneficial bacteria, and markers of inflammation; provides a detailed overview of gut microbiome health.
- Fecal calprotectin: Measures inflammation in the intestines; high levels indicate inflammatory bowel disease.
- Zonulin: Zonulin is a protein that regulates intestinal permeability. Elevated levels of zonulin in the blood can indicate increased intestinal permeability or “leaky gut,” which may be associated with various gastrointestinal and systemic conditions. Testing zonulin levels can help assess gut health and guide appropriate interventions.229
- Fecal occult blood test: Detects hidden blood in stool; can indicate gastrointestinal bleeding or conditions like colorectal cancer.
- Gastrointestinal pathogen panel: Detects bacteria, viruses, and parasites in the gut; helps diagnose infections causing gut issues.
- Lactulose breath test: Diagnoses small intestinal bacterial overgrowth (SIBO); measures hydrogen and methane produced by gut bacteria.
- SIBO breath test: Specialized breath tests are the most commonly used method for diagnosing SIBO. After a one-day preparatory diet, patients consume a glucose- or lactulose-containing solution. The breath is then analyzed for hydrogen, methane, and hydrogen sulfide gasses to identify SIBO and its subtypes:153
- Hydrogen-dominant SIBO: Characterized by elevated hydrogen levels in breath tests. This type is associated with symptoms such as bloating and diarrhea, often detected when hydrogen levels increase by at least 20 parts per million (ppm) from baseline within the first 90 minutes of the test.
- Methane-dominant SIBO (IMO): Identified by high methane levels during breath testing. Methane levels of 10 ppm or higher at any point during the test indicate this subtype. It is commonly linked with constipation and can exacerbate symptoms of IBS-C.
- Hydrogen sulfide-dominant SIBO: Characterized by elevated hydrogen sulfide (H2S) levels, which are diagnosed if H2S levels reach 3 ppm or more at any time during the test. This subtype is less common but can cause severe gastrointestinal symptoms.
- SIBO breath test: This test is used to diagnose different SIBO types by measuring hydrogen, methane, and hydrogen sulfide levels in breath samples. It involves consuming a lactulose or glucose solution and then collecting breath samples at intervals to analyze gas levels. The TrioSmart test helps determine the specific type of SIBO present, guiding appropriate treatment strategies.230
- Endoscopy: Visual examination of the digestive tract using a camera; helps diagnose structural problems and inflammation.
- Colonoscopy: Examines the large intestine for abnormalities; helps identify conditions like IBD, polyps, and cancer.
- Capsule endoscopy: Swallowed camera capsule that takes images of the small intestine; useful for detecting issues not visible with standard endoscopy.
- pH monitoring: Measures acid levels in the esophagus; used to diagnose gastroesophageal reflux disease (GERD).
- Urea breath test: Detects Helicobacter pylori infection, a common cause of ulcers and gut inflammation.
- Hydrogen breath test: Helps diagnose lactose intolerance and other carbohydrate malabsorption issues.
- Intestinal permeability test: Measures the ability of the gut lining to prevent unwanted substances from passing into the bloodstream.
- Parasite stool test: Identifies parasitic infections in the gut that can cause various gastrointestinal symptoms.
- Microbiome analysis: Analyzes the composition of the gut microbiome; provides insights into microbial diversity and potential imbalances.
Key Takeaways
- Maintaining gut health is important for overall wellness, as the gut influences digestion, immunity, and even mental health.
- Dysbiosis and leaky gut syndrome are conditions that disrupt gut balance and can lead to a range of health issues across multiple systems, including digestive, immune, skin, neurological, cardiovascular, metabolic, hormonal, and musculoskeletal systems.
- A balanced gut microbiome supports digestion, nutrient absorption, and a robust immune system while also influencing mood and cognitive functions through the gut-brain axis.
- Conversely, an imbalanced gut can contribute to chronic inflammation, autoimmunity, and a host of diseases, highlighting the need for a proactive approach to gut health.
- Healing and maintaining gut health involves ongoing diet and lifestyle adjustments, and sometimes targeted interventions.
- Utilizing tests in the Function Health membership and other diagnostic tools can provide insights into specific imbalances and guide appropriate treatments.
- Regularly incorporate gut-friendly practices, stay informed, and seek professional guidance to sustain optimal gut function and overall well-being.
- For a deeper understanding, explore peer-reviewed articles, expert books, and reputable health websites, and consult healthcare professionals specializing in gut health.
FUNCTION HEALTH IS A HEALTHCARE TECHNOLOGY COMPANY AND NOT A LABORATORY OR MEDICAL PROVIDER. ALL LABORATORY AND MEDICAL SERVICES ARE PROVIDED BY INDEPENDENT THIRD PARTIES. FUNCTION HEALTH DOES NOT OFFER MEDICAL ADVICE, LABORATORY SERVICES, A DIAGNOSIS, MEDICAL TREATMENT, OR ANY FORM OF MEDICAL OPINION, THROUGH OUR SERVICES OR OTHERWISE. FUNCTION HEALTH’S SERVICES ARE NOT A SUBSTITUTE FOR MEDICAL CARE, MEDICAL ADVICE, AND/OR A DETAILED DISCUSSION WITH YOUR PRIMARY CARE PHYSICIAN OR OTHER LICENSED PROVIDER. IF YOU HAVE ANY QUESTIONS REGARDING ANY LABORATORY RESULTS OR OTHER INFORMATION THAT YOU ACCESS THROUGH FUNCTION HEALTH, WE RECOMMEND THAT YOU DISCUSS THOSE QUESTIONS WITH A PRIMARY CARE PHYSICIAN OR OTHER LICENSED PROVIDER. ALL MATERIAL, INFORMATION, DATA, AND CONTENT THAT FUNCTION HEALTH PROVIDES IS STRICTLY FOR GENERAL INFORMATION PURPOSES.
WITHOUT LIMITATION, THE IDEAS AND INFORMATION PROVIDED IN THIS GUT HEALTH 101 GUIDE ARE STRICTLY FOR GENERAL INFORMATION PURPOSES AND DO NOT CONSTITUTE ANY FORM OF MEDICAL ADVICE OR A MEDICAL OPINION. EACH INDIVIDUAL, INCLUDING YOURSELF, PRESENTS A UNIQUE SET OF HEALTH REQUIREMENTS, RESTRICTIONS, LIMITS, AND OTHER NEEDS – IN ADDITION TO POTENTIAL ALLERGIES, AS WELL AS POSSIBLE CONTRAINDICATIONS WITH CURRENT MEDICATIONS – AND THIS GUT HEALTH 101 GUIDE DOES NOT ACCOUNT FOR THOSE INDIVIDUAL CIRCUMSTANCES. MOREOVER, SCIENTIFIC RESEARCH AND KNOWLEDGE ON THE TOPIC OF WEIGHT UNDERGO CONTINUOUS REASSESSMENT AND EVALUATION; FUNCTION MAKES NO WARRANTY REGARDING THE ACCURACY, RELIABILITY, EFFICACY, TIMELINESS, OR VALUE OF THE INFORMATION CONTAINED IN THIS GUT HEALTH 101 GUIDE. PLEASE CONSULT WITH YOUR PRIMARY CARE PHYSICIAN OR ANOTHER LICENSED MEDICAL PROVIDER BEFORE MAKING ANY CHANGES RELATING TO YOUR DIET, EXERCISE, SLEEP SCHEDULE, LIFESTYLE, MEDICATION REGIMEN, SUPPLEMENT INTAKE, AND/OR OTHER DAILY PRACTICES.
What could cost you $15,000 is $499
Function membership
$42
This is the most comprehensive lab testing I have ever had. I am thrilled to know more about my health and how to improve it.
Best money I have spent on healthcare.
Function blows my mind. The UI, UX, price and clinician notes are all phenomenal.
